RECOIL OFFGRID Preparation Masks and Respirators for Covid 19
In This Article
The COVID-19 pandemic has brought many changes to our lives. Among the most obvious is the routine use of protective masks to prevent spreading this disease. There has been much debate about the usefulness of masks, and official guidance has flip-flopped from discouraging to encouraging their use. Many are left wondering, can they help? What kind of mask do I need? Can I make my own? These are important questions right now, and they’ll remain relevant the next time a disease inevitably spreads like wildfire through the human population.
Face masks can prevent the spread of viral illness, including COVID-19, if the right type is used and used correctly. To understand how masks help, we must first understand transmission of the SARS-CoV-2 virus that causes COVID-19. The primary mechanism for transmission of the virus is droplets expelled from the body by coughing, sneezing, or breathing. The virus replicates in cells of an infected person, producing new copies of itself, which can then be shed in excretions such as saliva, mucus, phlegm, and rheum. Droplets of these bodily fluids can be distributed onto surfaces where they can be picked up by contact, but they can also be passed on through the air. When someone sneezes or coughs, expelled droplets can hang in the air for some time, or land directly in the nose or mouth of others. Viral particles in these droplets can then infect the recipient. The use of masks reduces this risk in two ways: Masks can contain these droplets when someone coughs or sneezes, and masks can protect the wearer from inhalation or intake of these droplets.

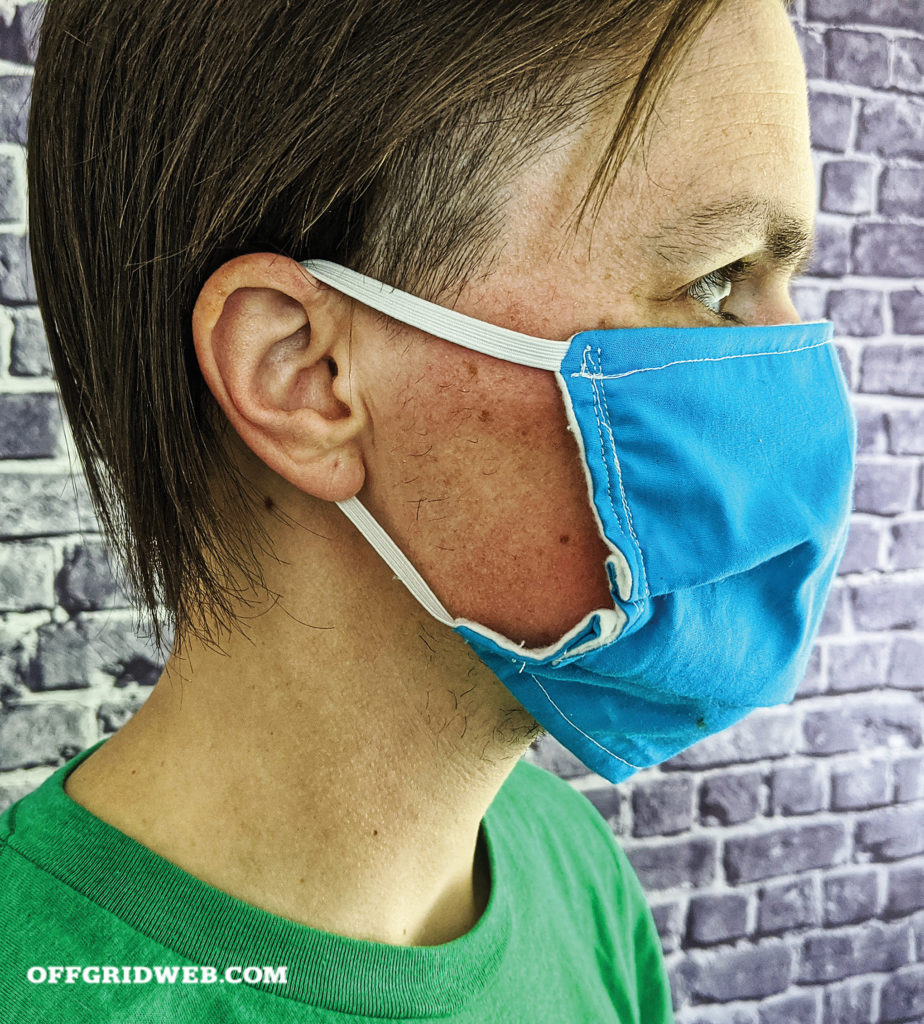
Above: Mask fit is an important consideration. Ideally, a mask should contour around the nose and cup the chin
Not all masks are equal. There are different types of masks sold for protection, but only some of them filter out dangerous pathogens. When searching for face masks, the results can be overwhelming. Respirators, N95, N99, PM2.5, surgical masks, dust masks — what are these things, and what are the differences?
Dust Masks: The most common type of face mask. This type of mask isn’t tested to any standard and is only for protection from large dust particles from cleaning, manufacturing, or craft processes.
Surgical Masks: The classic surgeon's mask. Loose fitting, allowing air to pass around the sides of the mask. Mostly a barrier against large droplets, splashes, and sprays. These masks are only used to prevent spread of droplets from the wearer. They don’t give protection to the wearer, only to others.

Above: A tin tie scavenged from a coffee bag serves as a malleable nose piece on our DIY mask.
Air Purifying Respirators: Close-fitting masks that force inhaled air through a filter to remove the smallest particles possible. The most common are N95 respirators, which filter out >95 percent of particles 0.3 micron or larger (and many that are smaller). Other grades, such as N99, filter out closer to >99 percent, while more specialized respirators such as P95 filter out >95 percent while being oil-proof as well.
Pollution Masks: Masks sold to protect the wearer from air pollution. These are uncommon in the United States but common elsewhere. Some are little more than a dust mask, while others are a washable fabric mask with disposable filter inserts. These masks are often marketed as PM2.5 masks, meaning they’re designed to filter pollution particles 2.5 microns in size or smaller. Many filters for this type of mask are N95 filters, but not all. It’s important to know which ones use which filters. Not all pollution masks fit well, which can greatly compromise effectiveness.
There are other respirators that enclose the face or use supplied air, but these are unlikely choices for most users. For reducing viral transmission among the population, simple face mask designs are more available, affordable, and easily made. The best are respirators that cover the nose and mouth, called half-mask filtering face-piece respirators (FFR). FFRs can come in different forms, such as classic disposable N95 masks or rubber masks with removable filters called elastomeric respirators. Elastomeric respirators can be impractical for daily wear outside of industrial environments, but much of what follows applies to them as well.

The ideal protection from SARS-CoV-2 is an N95 (or better) filtering face-piece respirator, that fits properly. Such respirators are made from a nonwoven synthetic material that carries an electrostatic charge. Nonwoven materials are a matrix of fine fibers in an irregular arrangement, which entrap particles as air passes through. The electrostatic charge attracts particles to the fibers, dragging them in and trapping them. It’s these properties that give N95 masks their ability to filter out even viruses.
Although the individual SARS-CoV-2 virions are about 0.1 micron in size, N95 respirators can entrap them. Filtration is measured against 0.3-micron particles, as these are the most difficult size to entrap. Larger particles are easily caught by many materials. Particles under 0.3 micron are subject to a phenomenon called Brownian Motion, which causes them to bounce off air molecules erratically. This erratic motion makes sub-0.3-micron particles easier to trap as they bounce into the filter. 0.3-micron particles are the most difficult, as their travel is less erratic and their size is small enough to pass many filters. A filter that can catch 0.3-micron particles in significant number, 95 percent or greater, is effective against both larger and smaller particles. This makes N95 and better the ideal choice here … with a couple of caveats. The respirator must have a tight fit to the face that doesn’t allow air around the edges of the mask. Both inhaled air and exhaled air must pass through the filter to offer protection. N95s that are vented offer no community protection if worn by an infected person. N95s that don’t fit the wearer allow both inhaled and exhaled air around the edges, offering no protection to anyone.
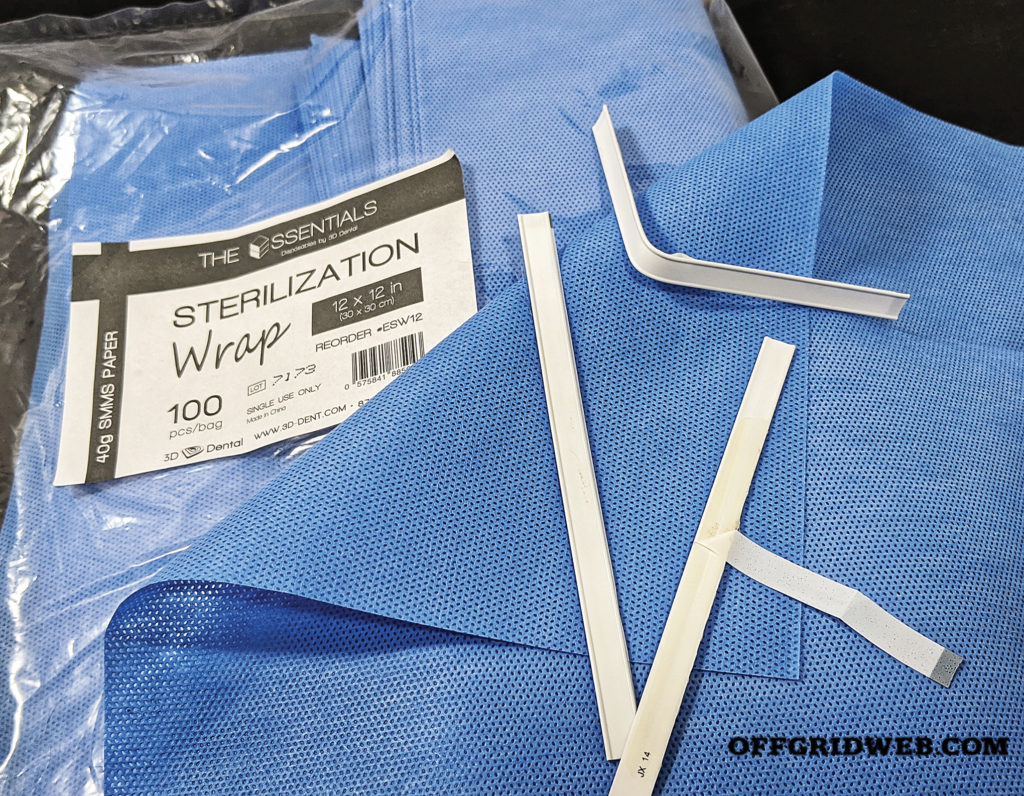
Above: Reasonably effective homemade masks can be constructed from sterilization wrap, a non-woven fabric used in hospitals.
In an ideal world, we would have enough N95s available for everyone. Unfortunately, they’re in short supply, if available at all, and are likely to remain so. Efforts are underway to extend the supply of N95s for healthcare workers, but despite this, many have had to find ways to do without. Similarly, most people outside healthcare have had to make do with other types of masks. For those who have the least resources, the only option has been fabric masks. According to the Centers for Disease control, the very last tier of acceptable masks are fabric, but can fabric masks actually work? The answer is yes and no.
Sadly, this situation has been long predicted by epidemiologists. Fabric masks have been studied, and science has some answers. We identified several scientific papers published since 2008 about fabric masks. Those studies looked at the usability and filtration of various fabrics, particularly cottons, for masks. From their findings, we can distill some best practices for fabric masks.
Cambridge University researchers found that some materials not only filter better, but can also fit better than others. They investigated various cotton materials and HEPA filter vacuum bags for both fit and filtration. While HEPA bags filter well, they don’t fit well if made into masks. Different weights and thicknesses of cotton fit better, but filtration varied. Double layers of tea-towel were found to have the best filtration. A single complete mask, of the surgeon’s mask style, made from T-shirt cotton was found to be somewhat effective at blocking particles expelled, but not effective at preventing their inhalation. Dutch researchers also studied masks made from layers of tea-towel, compared to surgical masks and N95s. All types of masks were found to reduce exposure to particles, but homemade were less effective than commercial styles. These researchers also looked at how wear affected the performance of homemade masks. They found that homemade masks were stable in the protection they offered for a few hours of wear at different activity levels.
Other studies measured common fabrics from garments like sweatshirts and T-shirts, finding that filtration varied widely, with none of the materials coming close to N95 masks in single layers. Leakage around the edges of homemade masks was determined to be likely, possibly owing to simple designs and the lack of sealing features. However, the resounding conclusion of the data is that fabric masks offer at least some protection when made from high-thread-count fabrics, particularly denser fabrics used in multiple layers. Other key factors identified were the use of dry masks, as moisture can compromise filtration, and the use of masks along with other preventative measures like hygiene and environmental sanitation.

Above: Masks should extend beneath the chin, but facial hair can impede their ability to seal in this area.
Another material option for homemade masks is nonwoven fabrics. Nonwovens are used in many roles, including masks and other filters for medical use. They’re more effective filters than woven material, and resist saturation by moisture. One nonwoven material in particular shows promise. When surgical instruments are sterilized, they’re bundled in a nonwoven fabric called sterilization wrap. This wrap stays in place after sterilization to maintain sterility by filtering pathogens in the environment. In response to N95 shortages, some doctors have turned to making masks from sterilization wrap. The lowest common grade of sterilization wrap provides >96 percent filtration against 0.3-micron particles in a single layer, and two layers could equal N99 performance.
It’s important to note, not all sterilization wrap is equal. Some sterilization wraps are made from cellulose, which can tear easily. The type to use for a face mask is made from polypropylene. This sterilization wrap is identified most often as SMS (Spunbond-Meltblown-Spunbond) or SMMS (Spunbond-Meltblown-Meltblown-Spunbond). This refers to how each layer of the material is made, either by being spun into erratic webs by air streams and then thermobonded (Spunbond), or by forcing molten polypropylene through tiny nozzles into air streams that mix the web, bonding as it cools (Meltblown). Meltblown is the primary filtering layer, but fragile. Spunbond is tough and tear resistant. Bonding them together creates a soft, breathable, moisture-repellent fabric with excellent filter properties and improved durability.
The question that remains is how to make an effective mask of these materials. There are many patterns for making masks at home, but some are worse than others. Many won’t protect either the wearer or those around them. Designs made with single layers of material, or the wrong type of material, won’t work. Designs that leave gaps around the nose, cheeks, or chin also won’t work. Anywhere air can get in around the edge, particles and droplets can get in or out. Many available designs give false confidence, rather than actual protection. Comparing several different patterns, we found the best designs are sewn with contouring to fit the user’s face. Surgical mask patterns that lay flat when not worn were the least successful, with a loose fit and less comfort. Not all contoured designs are equal, however, and some available patterns had to be adjusted to cup the chin or cover the nose. When selecting a pattern for making a mask, the design must extend over the bridge of the nose, and underneath the edge of the wearer’s chin, fitting tightly across both cheeks and all edges.
Other critical elements are formable nose pieces, and well-fitting attachments. Nose pieces that can be formed over the bridge of the nose are essential for proper sealing. Nose pieces can be made from copper wire — a short piece with rolled ends could be sewn into masks nose bridge, then bent into shape for wear. The downside is potential discomfort. The ideal solution we found is a packaging closure called a tin tie. Commonly found on coffee bags, these are a length of ¼-inch-wide plastic with two malleable wires in either edge. A 2.5-inch-length sewn into the bridge of the mask's nose is a comfortable and effective nose piece. How the mask is held to the face also affects fit and comfort. Commercial respirator designs use elastic straps that run behind the head, while surgical masks often use elastic loops over the ears or ties that go behind the head. Each can be adapted to homemade masks, but each has shortcomings. Dual elastics around the head are the most stable but can be difficult to size properly. Ties can slip and may not get tight enough. Ear loops are easiest to fabricate, but are uncomfortable for prolonged wear and will slip off some wearers’ ears. One solution for ear loops is to use 2mm round elastic hair ties to form the loops, which we found to be more secure and comfortable.

Above: A loose-fitting mask allows unrestricted airflow around the nose and cheeks, leading to higher risk of disease transmission.
Prolonged wear of ear loops can cause discomfort or even injury. Healthcare workers have reported irritation and wounds from ear loops after prolonged wear. A simple device called an ear saver can be fabricated to alleviate this. These devices connect the two loops across the back of the head, relieving pressure. Ear savers can also offer better adjustment of mask fit for variations in face shape. Many types of ear savers are being produced, from leather, die-cut plastic, and by 3D printing. The thermoplastic Kydex, commonly used in holster-making and hobbyist workshops, can quickly be turned into an ear saver. A ½-inch strip is cut, and each end heated then curled over to form a small hook. Sized between 2¾ and 3¾ inches, these can fit most users, tuning up mask fit and relieving pressure.
To get the most use out of any masks, we have to be able to reuse them. To reuse a mask, it must be decontaminated between uses. Mask decontamination has been studied, and COVID-19 has spurred many new efforts. Hospitals are exploring technology to meet demand, and the CDC has created decontamination guidelines. Unfortunately, many suggested methods are industrial solutions such as ultraviolet radiation and vaporous chemical disinfection and won’t work for individuals. Fortunately, there are other options. Plain, fabric masks can be washed using hot water and detergent, but masks from nonwoven materials cannot. The methods available to individuals are steam, dry and moist heat, and some chemical disinfection methods.
Masks can be steamed in the microwave or on the stovetop with appropriate steamers. Steam has been successful in studies but comes with risks. Higher temperatures can damage nonwoven materials, and microwaves should never be used for masks with metal components. Steam isn’t recommended for decontamination of N95s by their largest producer, 3M.

Above: A bag made of sterilization wrap keeps used masks isolated, and serves as a vessel during the decontamination process.
Dry heat decontamination, using the home oven, is more successful. Suspend masks, or place on a wooden rack, in the oven to prevent spot-heating from contact with metal racks. Masks should be baked at 160 to 175 degrees F for 30 minutes to allow the heat to fully penetrate. Many home ovens won’t go as low as 160 degrees F, but toaster ovens often go down to the safe 175 degrees F. If forced to use an oven that won’t go lower than 200 degrees F, the door can be cracked open to lower the temperature. Low heating remains detrimental, although the damage is low. Studies suggest this can be done 20 times before nonwoven materials are unacceptably degraded. Use an oven thermometer to ensure the temperature doesn’t exceed safe limits and use care. Handling contaminated masks in your home can spread particles, and the fan in many home ovens can blow particles off the mask before inactivation. This can be avoided by using a toaster oven that has no fan and can be set up in a closed garage or outside the home. Another solution is to fabricate a simple bag from sterilization wrap and drop masks carefully inside. The bag can then be closed and secured with a steel binder clip. That package can be inserted into the oven and baked appropriately.
Moist heat decontamination is similar to dry, but with the addition of evaporation, which is known to aid viral inactivation. The same temperatures as dry heat decon are used, but with the addition of a moisture reservoir. A 15- to 30-minute soak, at 50- to 80-percent humidity, is sufficient. Researchers have suggested a chamber for this — an enclosed container partially filled with water and a rack holding masks above the waterline. This container is put in the oven for the required time.

Above: Seal the mask during sanitation.
Disinfectant chemicals are another option, but many disinfectants effective against SARS-CoV-2 aren’t safe to use on masks. Both bleach and soap have been found to damage nonwoven materials. Alcohol destroys the electrostatic charge of N95s and other nonwovens, ruining their filtration ability. The safest disinfectant chemical to use on masks is hydrogen peroxide solution. In concentrations as low as <1 percent, hydrogen peroxide inactivates SARS-CoV-2 and is safe for use on nonwoven materials. Degradation of the mask will occur, and the 20-cycle limit seems to apply here as well.
The final method is time. Simply letting the mask sit in an isolated, dry, environment for over 72 hours is likely sufficient to inactivate SARS-CoV-2. Although fabrics and nonwovens haven’t been specifically tested, SARS-CoV-2 survives the longest on plastic and stainless steel, remaining viable for around 72 hours.
Whatever the decontamination method, strict procedures must be followed. Until decontaminated, masks and any container used for storing them are a transmission risk. Carelessness can spread viral particles and damage masks. Too many decontamination cycles can also damage masks. Institute procedures for identification and separation of clean and dirty masks, and for the handling, decontamination, and return to service of dirty masks. Label masks and use tally marks to track the decontamination cycles. Masks that have visible damage or have been heavily soiled by bodily fluids should be thrown away.
Masks cannot work to protect you or anyone if they aren’t worn properly. Masks must cover the parts of your face used to breathe: the mouth and nose. Masks also must seal tightly. You can’t have anything in the way of the seal. Facial hair, piercings, and dangling locks of hair can all break the seal.
In professional environments, regulations require individual fitting for respirators. If possible and if available masks are consistent in manufacture, fit testing should be performed using industry standard methods (see our gas mask buyer’s guide in Issue 26 for more details). This isn’t feasible for most of us, so it’s critical that every individual perform an informal seal check on every mask worn. To do this, first visually inspect the mask for damage. Put on the mask, adjust the nose piece, and ensure that edges of the mask are tight all around. With the mask in place, press your hands over it to block airflow and exhale fully. The mask should expand briefly before air escapes. Then, inhale fully. The mask should contract against the face, not pull air around the edges.
> Wash hands before handling, or donning, any clean mask.
> For N95 or other masks with dual elastics, cup the mask in your hand and place over your nose and mouth. With your other hand, pull the lower elastic over your head and below your ears. Repeat this with the upper strap, placing it above the ears.
> For a mask with ear loops, grasp by the loops, place the mask over the nose and mouth, and place the loops over each ear. If using an ear saver, hook one end of the device into an ear loop, hold it in place, and extend the other loop over the opposite end.
> For a mask with ties, grasp by the upper ties, place the mask over the nose and mouth, and secure the upper ties first and the lower second.
> Adjust the mask as necessary, tighten the nose piece, and seal check.
When doffing (removing) a mask, use extreme caution. The surface of the mask may have collected infectious particles. If you touch the surface, and then touch your face, you’ve defeated the entire purpose.

Above: It's not difficult to bend a scrap of Kydex into a DIY ear saver.
> Wash hands prior to removing your mask.
> Reach behind your head and grasp the elastics, ties, or clip securing your mask, unfasten them or stretch and lift them over the top of the head. If using a mask with ties or elastics that go around the head, remove the lower first, then the upper.
> Using the elastics/ties only, pull the mask off and away from your face.
> Avoid shaking or snapping your mask through the air, as this spreads particles.
> Handling it only by the elastics/ties, place the mask in paper or steriwrap bag, or other container, and close the container.
> Wash hands thoroughly again to remove any particles picked up from handling the mask.
> Remove a clean mask from storage, place and secure it on the face, and perform a seal check.
Clean masks should be stored in clean, dry, containers that prevent contamination. Masks should not be stored in containers that trap moisture, as this can degrade mask performance, and in the case of worn masks, can preserve pathogens.
Masks are only part of the solution. Hand hygiene, other forms of protective equipment as necessary, and overall hygienic practices are all essential. These things together can effectively reduce infection and transmission of any viral illness.
Don’t miss essential survival insights—sign up for Recoil Offgrid's free newsletter today!
Check out our other publications on the web: Recoil | Gun Digest | Blade | RecoilTV | RECOILtv (YouTube)
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments